Unfortunately, in the year since this Hormone Choice Singapore (HCS) website was started, the confusion about bioidentical hormone replacement therapy in Singapore has continued, creating a great deal of stress for patients who suddenly find their hormone treatment (including desiccated thyroid) no longer available or difficult to find and for doctors who are unsure whether they are going to be penalised if they continue to give the healthcare they know is of such great benefit to their patients.
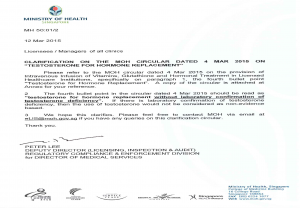
In March 2015 the Ministry of Health (MoH) sent two new circulars to Licensees/Managers of Clinics.
Testosterone For Hormone Replacement – eLis – Ministry
There was some confusion in the first circular in that none of the doctors consulted by HCS had heard of intravenous thyroid therapy being used for the conditions listed. The second circular containing a clarification of the first seemed to underline MoH’s own confusion. It is also not clear whether this guideline refers to synthetic or bioidentical testosterone hormone replacement.
In the second circular the second sentence in the second bullet is particularly interesting: “If there is laboratory confirmation of testosterone deficiency, then the use of testosterone would not be considered as non-evidence based”. In the opinion of both the doctors and patients HCS has spoken to, if this definition is followed, none of the bioidentical hormone replacement therapy used in
Singapore is non-evidence based, since all doctors who use it only do so with the guidance of regular laboratory blood tests. Indeed this is the joy of it, in that doses can be individually adjusted to reflect the tiniest change shown up in a blood test. This exact matching of the treatment to the individual patient is something that synthetic drugs cannot accommodate.
The circulars continue to call for “evidence based medicine”. One of the reference sources (Duke University, Introduction to Evidence-Based Medicine) on the MoH website gives us this definition from David Sackett, the founding father of the concept of evidence-based medicine (bolding by HCS):
Evidence Based Practice (EBP) is the integration of clinical expertise, patient values, and the best research evidence into the decision making process for patient care. Clinical expertise refers to the clinician’s cumulated experience, education and clinical skills. The patient brings to the encounter his or her own personal and unique concerns, expectations, and values. The best evidence is usually found in clinically relevant research that has been conducted using sound methodology.
(Sackett, D. (2002) Evidence-based Medicine: How to Practice and Teach EBM, 2nd edn. London: Churchill Livingstone.)
The Duke University website goes on (bolding by HCS):
The evidence, by itself, does not make the decision, but it can help support the patient care process. The full integration of these three components into clinical decisions enhances the opportunity for optimal clinical outcomes and quality of life. The practice of EBP is usually triggered by patient encounters which generate questions about the effects of therapy, the utility of diagnostic tests, the prognosis of diseases, and/or the etiology of disorders.
(The analysis below is taken from Evidence Based Practice, McGraw-Hill Education: https://www.mheducation.co.uk/openup/chapters/9780335244737.pdf )
Sackett acknowledges and values the different types of knowledge held by the clinician, for example, knowledge acquired through cultural and personal experiences, logical and critical knowledge gained through curriculum and the extra insight that can only be acquired through cumulative clinical expertise. He values the patient as an empowered decision maker and highlights that not all research is transferable into practice due to flaws in either design or reason.
Note that Sackett states that the best evidence is usually found in what the MoH would call “relevant research”. However, when the evidence found in laboratory tests is responded to with finely adjusted bioidentical hormone replacement (including desiccated thyroid) there is ample evidence available provided by well respected doctors worldwide (some of it on this site) that patients are receiving the care they need and, further, the care that addresses “the patient’s unique concerns, expectations, and values”.
Since bioidentical hormone therapy is derived from a plant source that cannot be patented, little money is likely to be made available for expensive studies to match those funded by drug companies who stand to make mega-bucks from any drug produced as a result. Nevertheless, those patients who continue to use the hormones all over the world constitute a huge body of “evidence” of their value, while well-run studies continue to point out the flaws, clinical and ethical, in synthetic hormone replacement therapy.
Share